
Non-Surgical Treatment of Rotator Cuff Tears: Evidence-Based Options for Healing and Recovery
Many rotator cuff tears can improve without surgery. Advances like Platelet-Rich Plasma (PRP) therapy, shockwave treatment (ESWT), and laser therapy now offer faster recovery, less pain, and better shoulder function. Learn how these evidence-based, non-surgical options support tendon healing and help athletes and active adults return to the activities they love.
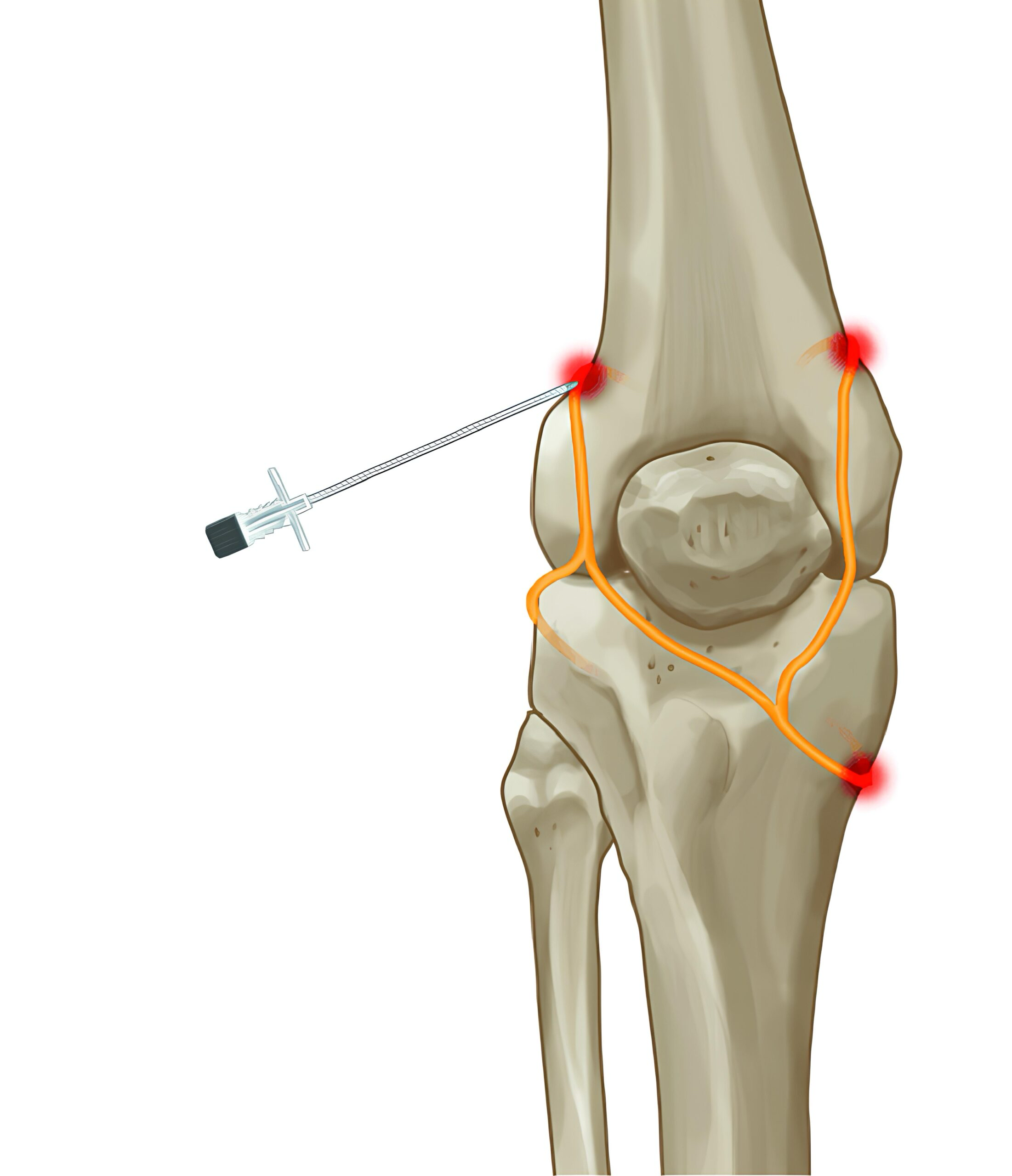
Intraosseous Orthobiologics: A New Frontier in Knee Osteoarthritis Care in Bend, Oregon
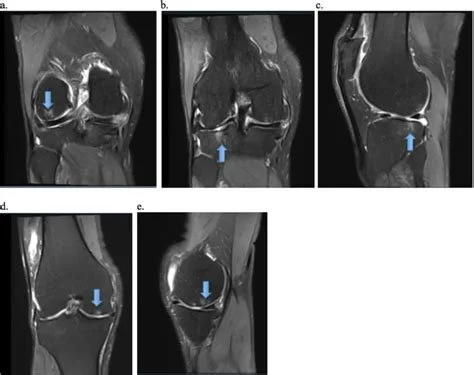
Typical MRI appearance of subchondral osteoarthritis-associated BML in the knee. Pasculli, Rosa & Kenyon, Charles & Berrigan, William & Mautner, Kenneth & Hammond, Kyle & Jayaram, Prathap. (2022). Mesenchymal stem cells for subchondral bone marrow lesions: From bench to bedside. Bone Reports. 17. 101630. 10.1016/j.bonr.2022.101630.

Is High-Dose Platelet-Rich Plasma (PRP) Better for Treating Knee Osteoarthritis?
Learn how high-dose platelet-rich plasma (PRP) therapy can provide better and longer-lasting relief for knee osteoarthritis compared to standard doses. Discover the benefits, safety, and what’s right for you.













Exercise as Medicine for Knee Arthritis
Personalized Sports Medicine, Interventional Orthopedics and Performance Medicine.
